Hospitals and maternity wards have COVID-19 protocols in place to protect you and your newborn. It’s important that you make any and all healthcare decisions with your doctor, including when you have coronavirus and it’s time to give birth to your baby.
The Centers for Disease Control and Prevention (CDC) is helping healthcare facilities that provide obstetric care, labor and delivery, recovery and inpatient postpartum care for pregnant patients with confirmed coronavirus or suspected of having the virus prepare for your labor and delivery. Here’s what you need to know:
When you have COVID-19 and it’s time to give birth
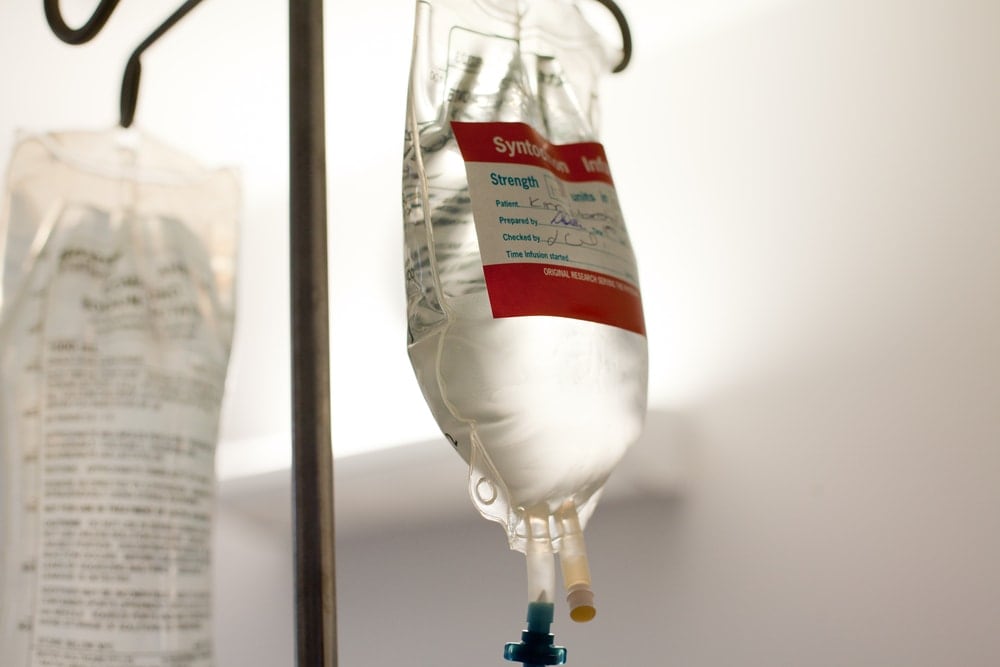
- Notify the hospital that it’s time for you to come in. Give them plenty of notice so they have the time they need to prepare for your arrival. This may include identifying the most appropriate room for labor and delivery; ensuring infection prevention/control supplies and personal protection equipment (PPE) are ready; and alerting your healthcare team about infection control requirements.
- If you need to be transported to the hospital by ambulance or other emergency medical services, alert the company (and 911 if you call them) so they can use good infection control and other protections. They will also remind the emergency room/maternity ward that you have or are suspected of having COVID-19.
If I have COVID-19, can I pass it to my baby during pregnancy or delivery?
According to a few reports, some newborns have tested positive for COVID-19. But that doesn’t necessarily mean they picked it up from their mothers in the womb. The most common way to get COVID-19 is through respiratory droplets that a sick person coughs or sneezes. Experts believe it’s more likely that infected babies picked it up through droplets after birth from their mother or a caregiver.
What to expect during delivery
There’s no evidence that women with COVID-19 shouldn’t deliver vaginally. But delivery might be different from what you expected.
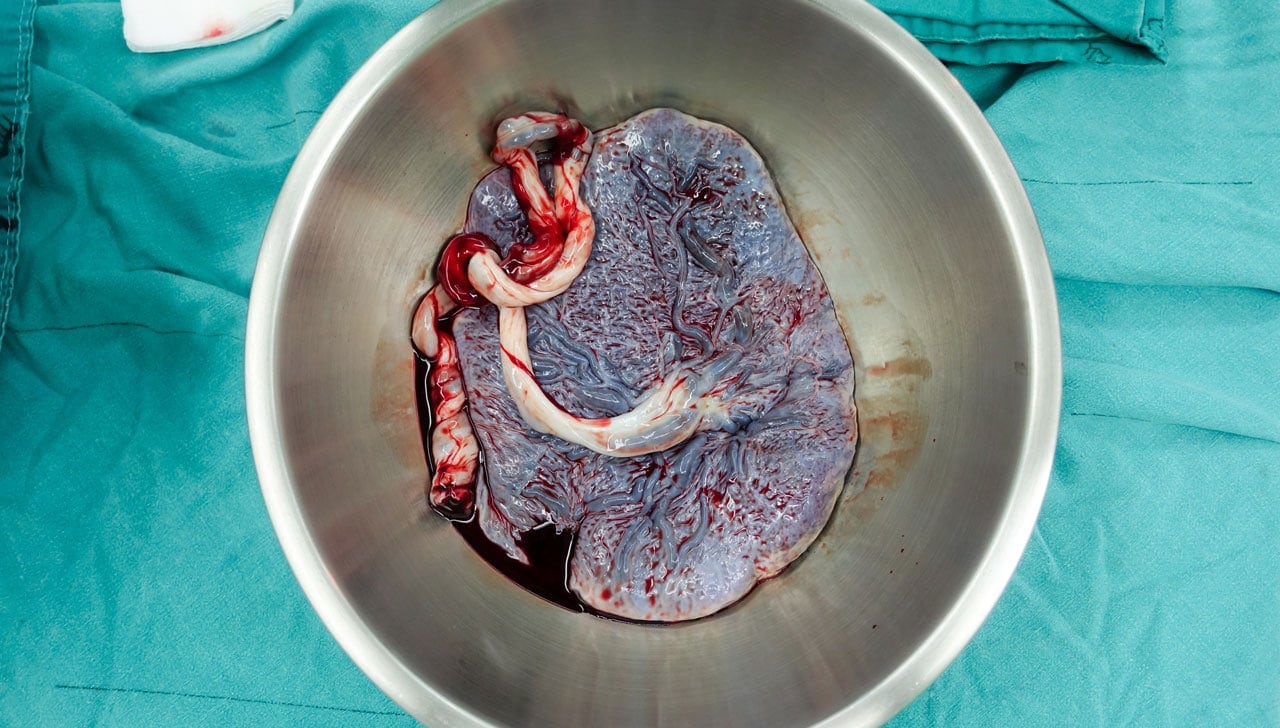
One group of experts suggests that if the mother has COVID-19, it might be helpful to leave the vernix — a white, waxy coating on newborns’ skin — on for 24 hours after birth. The coating contains antimicrobial substances that could protect against infection.
During Hospitalization
The American College of Obstetricians and Gynecologists recommends that babies born to women who have the coronavirus be isolated and monitored for symptoms.
- You will likely be placed in a single-person room with a dedicated bathroom. The door should remain closed.
- Your healthcare team will employ the CDC’s standard and advanced precautions for infection prevention and control. This may include asking you to wear a face mask to prevent transmission to others, including your infant. The team will wear respirators or face masks, gowns, gloves and eye protection (PPE). These protection items should be put on before entering your room and after leaving your room.
- Healthcare teams caring for infants born to mothers with confirmed COVID-19 will exercise the same cautions and procedures.
- Visitors will be restricted and encouraged to use alternatives such as video-call apps on cell phones or tablets. If visitation must occur, the hospital may require visits to be scheduled and controlled, plus:
- Visitors will be screened for fever and respiratory symptoms. Also for underlying illness putting them at higher risk for COVID-19) and ability to comply with precautions.
- Facilities may provide instruction, before visitors enter patients’ rooms, on hand hygiene, limiting surfaces touched, and use of personal protection equipment while in the patient’s room.
- Visitors should not be present during specimen collection procedures.
- Visitors will be allowed to only visit the patient room. They should not go to other locations in the facility.
Mother/Baby Contact
According to the CDC, the virus that causes COVID-19 is thought to spread mainly by close contact with an infected person through respiratory droplets. Whether a pregnant woman with COVID-19 can transmit the virus that causes COVID-19 to her fetus by other routes of vertical transmission (before, during, or after delivery) is still unknown.
However, in limited recent case series of infants born to mothers with COVID-19, none of the infants have tested positive for the virus that causes COVID-19. Additionally, the virus was not detected in samples of amniotic fluid or breast milk.
There’s no evidence that the virus itself can lead to birth defects, miscarriage, or any other problems. But a fever in early pregnancy, from COVID-19 or any other cause, can raise the chances of birth defects. And severe lung illnesses late in your pregnancy can make you more likely to deliver your baby prematurely. Some babies born to women who had coronavirus were born preterm. But it’s not clear whether the virus was to blame.
Because it is unknown if a pregnant woman with COVID-19 can transmit the virus to her baby before, during or after delivery, the hospital will likely take extra precautions to avoid any potential complications. These may include
-
- Temporarily separating (e.g., separate rooms) mothers who have or are suspected of having COVID-19 from her baby until the mother’s symptoms clear.
- The risks and benefits of temporary separation of the mother from her baby should be discussed with the mother by the healthcare team.
- A separate isolation room should be available for the infant while they remain a PUI (person under investigation). Healthcare facilities could limit visitors, with the exception of a healthy parent or caregiver. Visitors will be instructed to wear gown, gloves, face mask, and eye protection (PPE). If another healthy family or staff member is present to provide care (e.g., diapering, bathing) and feeding for the newborn, they should use gowns, gloves, face masks, and eye protection.
- The decision to discontinue temporary separation of the mother from her baby will likely be made on a case-by-case basis in consultation with clinicians, infection prevention and control specialists, and public health officials. The decision should take into account disease severity, illness signs and symptoms, and results of laboratory testing for the virus that causes COVID-19.
- If it’s necessary that the newborn stay with his/her ill mother in the same hospital room, the hospital will take measures to reduce exposure of the newborn to the virus that causes COVID-19:
- Physical barriers (e.g., a curtain between the mother and newborn) and keeping the newborn at least 6 feet away from the ill mother.
- If no other healthy adult is present in the room to care for the newborn, a mother who has confirmed COVID-19 or is a PUI should put on a face mask and practice good hand hygiene before each feeding or other close contact with her newborn. The face mask should remain in place during contact with the newborn.
Breastfeeding with COVID-19
- During temporary separation, mothers who intend to breastfeed should be encouraged to express their breast milk to establish and maintain milk supply. If possible, a dedicated breast pump should be provided. Prior to expressing breast milk, mothers should practice hand hygiene. After each pumping session, all parts that come into contact with breast milk should be thoroughly washed and the entire pump should be appropriately disinfected per the manufacturer’s instructions. This expressed breast milk should be fed to the newborn by a healthy caregiver.
- If a mother and newborn do room-in and the mother wishes to feed at the breast, she should put on a face mask and practice hand hygiene before each feeding.
All information is from the Centers for Disease Control and Prevention.