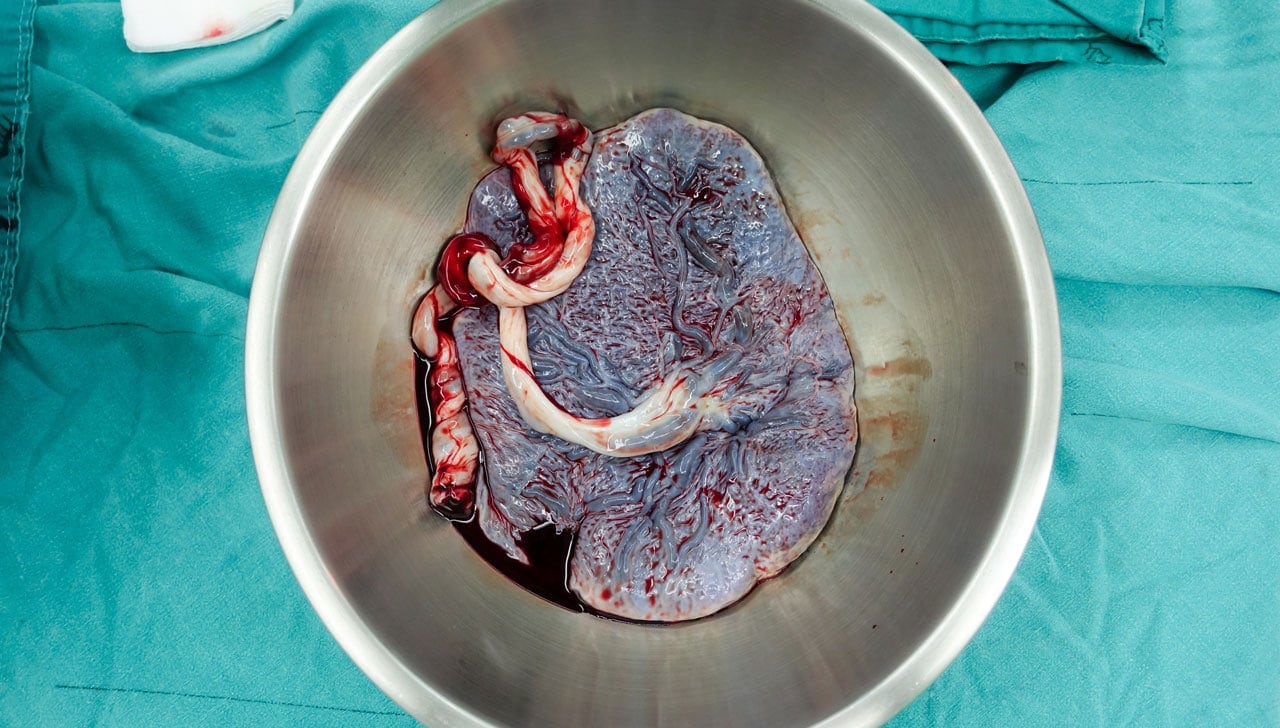
The final stage of labor occurs when the placenta is expelled from the mother’s uterus. For many women, this process happens on its own after the baby has come through the birth canal. However, for some, this process doesn’t happen automatically, resulting in a phenomenon called retained placenta.
What Is a Retained Placenta?
Labor takes place in three stages:
- The first stage of labor begins with contractions that indicate that the uterus is preparing to deliver a baby.
- Once a woman has given birth, the second stage of labor is complete.
- The final stage of labor takes place when the placenta is expelled from the woman’s womb. This stage usually takes place within 30 minutes of the baby’s birth.
However, if the woman has not expelled the placenta after 30 minutes of delivery, this is considered a retained placenta. If a retained placenta is not treated, the mother is susceptible to both infection and extreme blood loss, which could be life-threatening.
Two Approaches to Delivering the Placenta
If your pregnancy has moved through the labor and birth stages normally, you can choose how to handle the final stage of labor. This process is usually a part of a woman’s birth plan discussion.
There are generally two approaches used when dealing with the placenta, whether a natural approach or a managed approach.
- A natural approach allows the woman’s body to naturally expel the placenta on its own.
- Medical personnel assists the managed approach and usually, occurs when a shot is administered to the thigh while the baby is being born to cause the woman to expel her placenta.
Syntometrine, ergometrine, and oxytocin are the drugs used to cause a woman’s body to contract and push out the placenta. If a woman has had complications like high blood pressure or preeclampsia during her pregnancy, Syntocinon is given.
The benefit of opting for a managed final stage of labor is the reduction in bleeding immediately after the baby is born.
Three Types of Retained Placenta
- Placenta Adherens: occurs when the contractions of the womb are not robust enough to completely expel the placenta. This results in the placenta remaining loosely attached to the wall of the uterus. This is the most common type of retained placenta.
- Trapped Placenta: is when the placenta successfully detaches from the uterine wall but fails to be expelled from the woman’s body it is considered a trapped placenta. This usually happens as a result of the cervix closing before the placenta has been expelled. The Trapped Placenta is left inside the uterus.
- Placenta Accreta: is when the placenta attaches to the muscular walls of the uterus instead of the lining of the uterine walls. Delivery becomes more difficult and often results in severe bleeding. Blood transfusions and even a hysterectomy may be required.
What Causes a Retained Placenta?
- Placenta Percreta occurs when the placenta grows all the way through the wall of the womb.
- Uterine Atony occurs when a woman’s contractions stop or are not strong enough to expel the placenta from her womb.
- Adherent Placenta takes place when all or part of the placenta is stuck to the wall of the woman’s womb. In rare situations, this happens because the placenta has become deeply embedded within the womb.
- Placenta Accreta takes place when the placenta has become deeply embedded in the womb, possibly due to a previous cesarean section scar.
- A Trapped Placenta results when the placenta detaches from the uterus but is not delivered. Instead, it becomes trapped behind a closed cervix or a cervix that has partially closed.
A midwife can help prevent a retained placenta on rare occasions by gently pulling on the umbilical cord. However, the cord may break if the placenta hasn’t completely separated from the uterine walls or if the cord is thin. If this happens, delivery of the placenta can take place by using a contraction to push it out.
What Are the Signs and Symptoms of a Retained Placenta?
The most obvious sign of a retained placenta is when the placenta fails to be completely removed from the womb an hour after the baby’s delivery. Other symptoms may include:
- fever
- a foul-smelling discharge from the vaginal area
- large pieces of tissue coming from the placenta
- heavy bleeding
- pain that doesn’t stop
Who Is At Risk for a Retained Placenta?
Certain factors increase the likelihood of a woman experiencing a retained placenta.
They include:
- A pregnancy that occurs in women over the age of 30
- Having a premature delivery that takes place before the 34th week of gestation
- Experiencing an extremely long first and second stage of labor
- Delivering a stillborn baby
How Is a Retained Placenta Treated?
The treatment for a retained placenta is simply the removal of the placenta from the woman’s womb. Different methods to achieve this include:
- A doctor may attempt to remove the placenta manually. However, this does carry some risk of infection.
- Medications that relax the uterus to make it contract can also be used to help expel the placenta from the womb.
- Breastfeeding can be utilized in some situations because the process causes the uterus to contract and may be enough to expel the uterus from the womb.
Sometimes, something as simple as urinating is effective enough to expel the placenta because a full bladder can sometimes get in the way of expelling the placenta from the womb.
Unfortunately, if none of these methods succeed in removing the placenta from the uterus, emergency surgery may be needed as a last resort. This is usually saved as the last approach because of the complications that surgery can create.
What Are the Potential Complications of a Retained Placenta?
The risk of heavy bleeding increases. This condition is referred to as primary postpartum hemorrhage (PPH). When the managed delivery of the placenta takes longer than 30 minutes, heavy bleeding often results.
You do have the option of requesting a general anesthetic, but you incur more risks, especially if you want to breastfeed right after the procedure. Traces of the drug will still be in your system which means the drug would also be in your breastmilk. You also need to make sure that you are alert enough to hold and support your baby for breastfeeding firmly.
However, if you do opt for the anesthetic, the placenta and any other remaining membranes will be manually removed from your womb while your legs rest in stirrups in the lithotomy position. After the procedure, you will be given antibiotics intravenously to avoid the risk of infection. Additional drugs will be given to help your womb to contract afterward.
What Is the Outlook for Women with a Retained Placenta?
A retained placenta can be treated. Timing is everything. The sooner steps are taken to rectify the problem, the better the outcome.
If you fall into a high-risk category for a retained placenta or have experienced one in the past, talk to your doctor before giving birth again. Your doctor will help you prepare for the possibility of complications.
Can I Prevent a Retained Placenta in My Next Pregnancy?
Your chances of having a retained placenta increase after you’ve already had one. But, you can still have a healthy pregnancy that doesn’t produce this type of complication.
If your child is born premature, the risks increase as well. The placenta is supposed to stay in place for 40 weeks. As a result, premature labor may lead to a retained placenta.
Doctors do everything in their power to prevent a retained placenta by taking actions that hasten complete delivery of the placenta after the birth of the baby.
These steps are as follows:
- Medication that encourages contractions in the uterus to help push out the placenta. Oxytocin (Pitocin) is an example of a medication that might be used
- Control Cord Traction (CCT) after the placenta has released
- Stabilizing your uterus by applying CCT through touch manual touch
These are all standard steps that your doctor may perform before you deliver the placenta. After childbirth, your doctor will also recommend massaging your uterus to encourage contractions that stop the bleeding and allow the uterus return to return to a small size.
In the unfortunate event that your cord snaps or your cervix closes too quickly after the oxytocin injection, consider a physiological third stage if you conceive again.
If you allow the placenta to deliver naturally, the cervix will more than likely close at the appropriate time, instead of closing too quickly. Discuss your options with your doctor.
However, keep in mind that the prolonged use of Syntocinon (artificial oxytocin) during labor has contributed to retained placentas.
This concern may develop if your labor is induced or sped up. However, although the potential for having a retained placenta with future pregnancies is prevalent, it’s not a guarantee that you won’t have a healthy pregnancy and delivery.
Want to Know More?
Compiled using information from the following sources:
1. Begley C. 2014. Physiology and care during the third stage of labor. In: Marshall JE, Raynor MD. eds. Myles Textbook for Midwives 16th ed. Edinburgh: Churchill Livingstone, 395-416.
2. BMagann EF, Lutgendorf MA, Keiser SD, et al. 2013. Risk factors for a prolonged third stage of labor and postpartum hemorrhage. South Med J 106(2):131-5.
3. Coviello, E. M., Grantz, K. L., Huang, C. C., Kelly, T. E., & Landy, H. J. (2015, July 28). Risk factors for retained placenta.
4. Mayo Clinic Staff. Placenta: How it works, what’s normal.
https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/placenta/art-20044425
5. Use of nitroglycerin to deliver a retained placenta.
https://www.cochrane.org/CD007708/PREG_use-nitroglycerin-deliver-retained-placenta
6. Weeks, A. Retained placenta after vaginal birth.
https://www.uptodate.com/contents/retained-placenta-after-vaginal-birth